Enhancing the safety of virus-inactivated ancillary materials through neutralizing antibodies
The discovery of antibodies in the late nineteenth century marks one of the most significant advancements in our understanding of the human immune system. It catalyzed over a century of rapidly evolving investigations and characterizations of the invisible biochemical mechanisms that keep us safe every day. This blossoming immunological understanding continues to progress alongside our investigation into and characterization of the viruses and pathogens that plague human and animal populations.
In today’s world, over a year into the global COVID-19 pandemic, many are comfortable hearing terms like “antibodies,” “antigens,” and “immunity,” but the breadth and sophistication of the humoral immune system may not always be fully appreciated. Even in a healthy state, our blood and tissue fluids are infused with antibodies ready to specifically bind to an unfathomable number of unique biomolecules. This humoral immune feature becomes critically important when faced with invading pathogens. These first-line antibodies and the memory B cells selected to respond to these invading pathogens launch an explosion of activity that results in various outcomes depending on the effective mechanisms for the specific antibodies involved.
Main Functions of Antibodies
The three main functions of antibodies are known to be opsonization, complement activation, and immune neutralization.1 Opsonization is the process of tagging a pathogen to be detected and phagocytized by cells such as macrophages. An effective location for opsonization antibody attachment is dependent on being accessible and recognizable by phagocytic cells.2 The complement pathway is an innate system of proteins and signal molecules that can trigger inflammation, phagocytic action, and the rupturing of bacterial cells. Like opsonization, antibody-mediated complement activation is dependent on the bound antibody being accessible to the recruitable complement pathway initiation molecules.3 Immune neutralization results when a bound antibody interferes with an essential function of its target antigen molecule, neutralizing the normal effect of the target. Mechanisms of immune neutralization differ but include static interference4 and conformational changes.5
Immune Neutralization
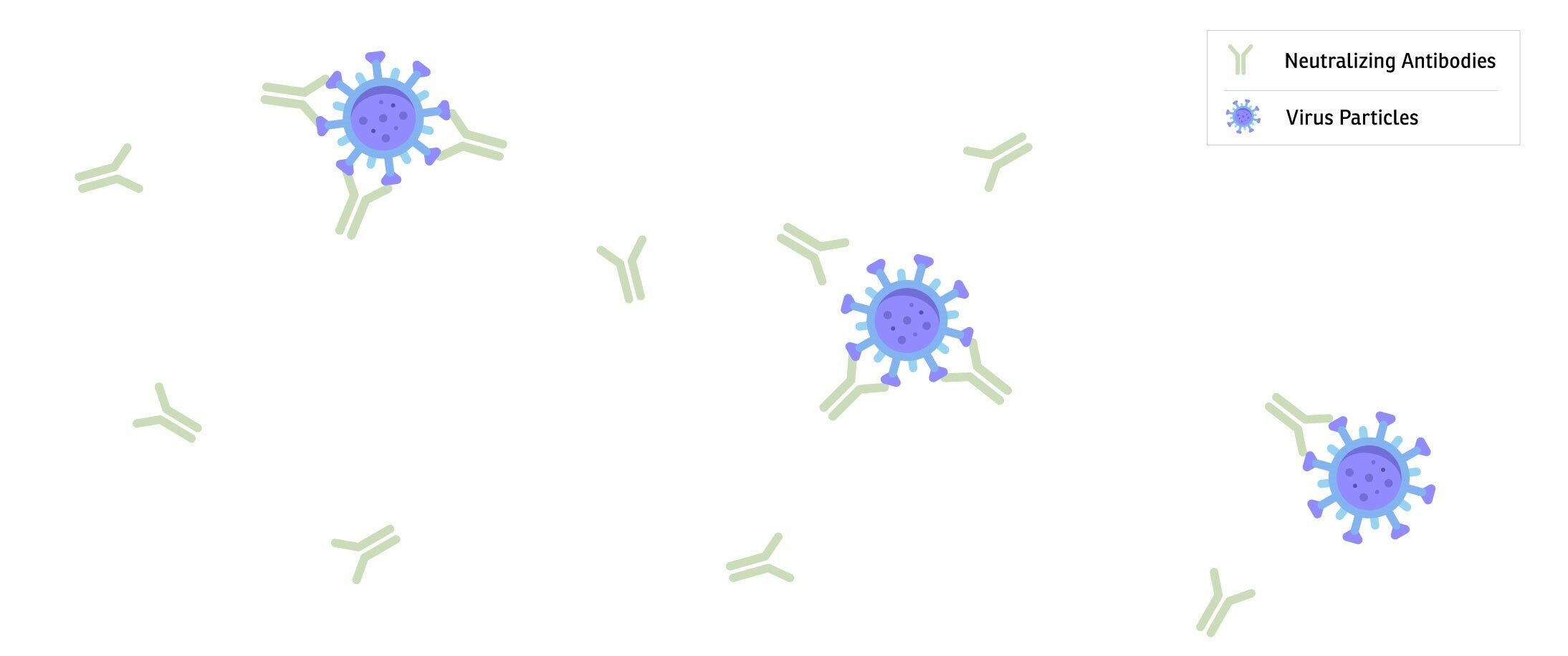
Immune neutralization has been a powerful ally for humans attempting to understand and fight infectious diseases. Antiserums containing neutralizing antibodies against viruses and bacteria have been used since the early twentieth century and are still being used today, e.g., against the Ebola6 and SARS-CoV-27 viruses. Once someone has been infected and recovers from a pathogen, their body fluids (blood plasma) will contain antibodies specific to that pathogen. This convalescent plasma can be collected and infused into another person sometimes creating what is known as passive immunity; it is possible for the neutralizing antibodies present in this antiserum to provide both effective prophylaxis against their target and a therapeutic intervention. This same neutralization phenomenon is responsible for what has been achieved via purified antibodies and monoclonal antibody production technology.8
In the age of purposefully engineered immune cells, we find immune neutralization working to our benefit again within some of the ancillary materials currently available that support these advanced cellular therapies. Akron has recently launched a global partnership with Octapharma to provide the advancedtherapy market with a virus inactivated human serum to be used as a safe and effective media supplement, helping to produce optimal end drug products while overcoming regulatory hurdles in the pathway towards commercialization.9 This new virus inactivated human serum product is made from an FDA-approved pharmaceutical product intended for human infusion (Octaplas®), which undergoes a robust solvent detergent treatment and benefits from immune neutralization through the pooling of 630 to 1,520 single donor units. This results in a significant reduction of enveloped and non-enveloped viruses.
Since the validated virus and pathogen reduction methods used in Octaplas® have already been approved by the FDA, drug and biologic manufacturers can move forward with confidence knowing the material they incorporate into their manufacturing process is maximizing the ultimate safety profile for the end user. The consistency achieved through the pooling of so many donor units also enables greater control over a therapy’s manufacturing process than conventional human-derived media supplements.
Furthering this consistency is immune neutralization and dilution of harmful interfering biomolecules. As an infusible drug product, Octaplas® minimizes the risk of a leading cause of transfusion-related deaths in the US — Transfusion-related acute lung injury (TRALI).10 A large numer of TRALI cases have been shown to be connected to the harmful antibodies Anti-HLA and Anti-HNA.11,12 It is suspected that this superior clinical result from Octaplas® is due to a combination of the dilution, immune neutralization, and filtration of these and other harmful biomolecules. Despite comprising both male and female donations, this reduction in immunization risk is also seen with the absence of anti-D immunization and the total lack of inhibitor formation during clinical trials.13
Conclusion
Given the safety and immunological advantages of Octaplas® over other conventional plasma options and the fact that more than 13.5 million bags have been transfused into more than 4.5 million patients worldwide across multiple indications14, Octaplas® presents itself as one of the best materials in the world to produce virus inactivated serum for use in the cellular therapy industry. Akron Biotech’s long history of manufacturing cGMP-compliant human serum and blood products enables us to leverage this new partnership to offer a superior product (Human AB Serum, Converted from Octaplas®, Pooled Plasma (Human), Xeno-Free, Virus Inactivated) while advancing the safety and standardization of the industry. This commitment to deliver top quality ancillary materials for use in the development of your final therapeutic exemplifies Akron’s mission to support the success and commercialization of tomorrow’s medicines.
References
- Huber M, Trkola A. Humoral immunity to HIV-1: neutralization and beyond. J Intern Med. 2007 Jul;262(1):5–25.
- Jones KF, Fischetti VA. The importance of the location of antibody binding on the M6 protein for opsonization and phagocytosis of group A M6 streptococci. J Exp Med. 1988 Mar 1;167(3):1114–23.
- Goldberg BS, Ackerman ME. Antibody-mediated complement activation in pathology and protection. Immunol Cell Biol. 2020 Apr;98(4):305–17.
- Zheng Q, Jiang J, He M, Zheng Z, Yu H, Li T, et al. Viral neutralization by antibody-imposed physical disruption. Proc Natl Acad Sci. 2019 Dec 26;116(52):26933–40.
- Roguin LP, Retegui LA. Monoclonal Antibodies Inducing Conformational Changes on the Antigen Molecule. Scand J Immunol. 2003 Oct;58(4):387–94.
- Use of convalescent whole blood or plasma collected from patients recovered from Ebola virus disease. WHO Technical Document; WHO/HIS/SDS/2014.8, 2014 Sep 14
- Convalescent Plasma. NIH COVID-19 Treatment Guidelines. 2020 Oct 9. https://www.covid19treatmentgu...
- Salazar G, Zhang N, Fu T-M, An Z. Antibody therapies for the prevention and treatment of viral infections. Npj Vaccines. 2017 Dec;2(1):19.
- Akron Biotech signs exclusive global agreement with Octapharma to produce virally inactivated human AB serum derived from Octaplas® for the cell therapy market. Octapharma Press Release. 2021 Jan 20 https://www.octapharma.com/new...
- Bertolini J, Gross N, Curling J, eds. Production of Plasma Proteins for Therapeutic Use. Hoboken, NJ; John Wiley & Sons; 2013: 345-351.
- Sachs UJH, Wasel W, Bayat B, Bohle RM, Hattar K, Berghöfer H, et al. Mechanism of transfusion-related acute lung injury induced by HLA class II antibodies. Blood. 2011 Jan 13;117(2):669–77.
- Curtis BR, McFarland JG. Mechanisms of transfusion-related acute lung injury (TRALI): Anti-leukocyte antibodies: Crit Care Med. 2006 May;34(Suppl):S118–23.
- BLOOD PRODUCTS ADVISORY COMMITTEE. Pooled Plasma (Human), Solvent/Detergent Treated (Octaplas™). BLA 125416/0. 2012 Sep 20.
- Octapharma. Data on file; 2013.